Both Germany and France have now suspended the marketing of Actos (pioglitazone) due to concerns of a link between Actos and bladder cancer. Though we have known about bladder cancer concerns for some time, these recent concerns about the bladder cancer link stem from a recent report analyzing the FDA's Adverse Event Reporting System (AERS), which found that 93 cases of cancer were recorded between 2004 and 2009 in patients treated with antidiabetic drugs of which 31 patients were treated with pioglitazone, representing a statistically significant increased risk of bladder cancer (ROR 4.30, 95% CI 2.82-6.52; p<0.0001). Interestingly, the FDA announced that it was going to look into the link between Actos and bladder cancer only a few days before it made it's final decision on what to do with Avandia (as if they didn't know about the Actos cancer risk before the July 2010 advisory board).
Despite the many things you have heard about Avandia, back in July 2010, the FDA decided to severely restrict the use of Avandia for three reasons:
1. Despite limited and conflicting data, there seemed to be a signal of myocardial infarction for patients taking Avandia.
2. The one study proving Avandia's safety, RECORD (see here for more details) was discredited by FDA scientists due to potential reporting errors.
3. The advisers on the panel felt strongly that despite limited and conflicting evidence, the signal was enough to be concerned AND because Actos (similar drug in same class) did not seem to show this signal, why would doctors ever want to prescribe Avandia?
I have blogged extensively about Nissen's meta-analysis that triggered the whole Avandia scare. Meta-analysis have major limitations. Another group of researchers using the same data as Nissen's with different statistical techniques concluded that Avandia did not cause heart attacks. Large, randomized trials are the only way to determine certainty, and all available large trials (DREAM, ADOPT, ACCORD, etc.) with rosiglitazone showed no heart attack risk. As mentioned above, the one study designed to definitively show whether or not Avandia led to cardiovascular risk (RECORD, which showed that Avandia did not cause cardiovascular risk, and in fact surpasses the FDA's standard for cardiovascular safety) was harshly criticized by those within the FDA that wanted to see Avandia pulled from the market. Specifically, the FDA found that GSK had some errors in reporting the results of RECORD. Though these types of errors are not uncommon in very large trials, and likely won't affect the overall results of the study, nonetheless, the deserve looking into. However, the FDA promised to do a complete independent analysis of the RECORD results; a promise it has yet to deliver on.
The main issue here is #3: Actos appears to be safe, so let's dump Avandia. (Interestingly, independent cardiologists analyzed all the data and did not find a conclusive difference in cardiovascular risk between Actos and Avandia). Here is the full transcript of the advisory board. Since it is a very difficult document to read through, I have pasted some of the direct quotes below from some of the advisers who voted to either remove Avandia from the market or severely restrict its use. Based on these quotes, I feel pretty strongly that had the advisers known about Actos' bladder cancer risk, that they may have voted very, very differently. However, the FDA did know about the association between Actos and bladder cancer. They just chose not to mention it! In fact, when one adviser brought up the question at the July advisory board, the FDA only briefly mentioned this and discussed it more as a class effect also seen with dual PPAR agonists.
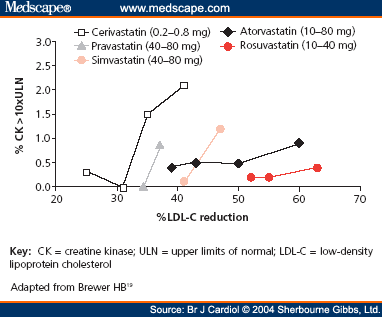
Avandia and Actos help diabetics use their own insulin better by hitting a receptor called PPAR. There are three main PPAR receptors: Alpha, Gamma and Delta. We don't know a whole lot about delta, but PPAR Gamma works on glucose, and PPAR alpha affects cholesterol. Fibrates like gemfibrozil, which lower triglycerides and raise HDL or good cholesterol are PPAR alpha agonists. Dual PPAR agonists were drugs that pharma were trying to develop that hit both alpha and gamma in order to help both with lipids and glucose. They have not been able to make it to market due to safety concerns (raised by, guess who??? Dr. Nissen). One of the differences between Actos and Avandia, is that Actos has a higher affinity for the PPAR alpha receptor, which is why it likely does a better job on raising HDL and lowering triglycerides than Avandia. Some have hypothesized that this might be the reason why Actos might not have the same cardiovascular issues as Avandia (though this has yet to be shown). If in fact, as stated during the FDA meeting (I am not aware that this data is published) that the bladder cancer risk was seen in both Actos and the dual PPAR agonists. Bladder cancer has not been seen with Avandia. In other words, the evidence (both available and suggested by FDA quotes that are public record) suggest that Actos may have more of a bladder cancer risk than Avandia.
Why the FDA in discussing to keep Avandia on the market would not extensively discuss the concerns of bladder cancer with Actos, paired with the weak and controversial data showing Avandia's cardiovascular risk and effort to discredit GSK's study proving Avandia's safety leads me to believe that the FDA's attack on Avandia was very much politically motivated. Scientists look at all the available data and weigh the risks and benefits of all options before making a conclusion. It is clear to me that the FDA's decision on severely restricting Avandia was more political then science. Based on the currently available data which now include bladder cancer risk, Avandia may actually be a better choice than Actos, but the FDA's restriction will essentially prevent any doctor from being able to prescribe Avandia after November.
Select quotes from advisers who voted to voted to either remove Avandia from the market or severely restrict its use:
DR. SCHAMBELAN: This is Morrie Schambelan. I voted E. (remove Avandia from the market) . I was one of the brain-dead kangaroos last time (meeting in 2007) who was on the fence, largely because I did see a signal for harm. I was led at that time by the comparison to active comparators, which I think is much more relevant to me than placebo. I wasn't swayed by the pioglitazone data that were presented at that time because they were pretty preliminary. I was much more persuaded this time, including Dr. Graham's analysis. I feel that pioglitazone is a perfectly acceptable alternative.
DR. SAVAGE: Peter Savage. I voted D (keep on the market with restrictions) I was also oscillating between D and E because I think that the evidence of potential harm associated with rosiglitazone is stronger now than it was in 2007. And very importantly, the evidence about pioglitazone is substantially greater than what we saw treat in 2007.
DR. FLEMING: Fleming. I voted E. My main sense about this is really explained in my answer to question number 7. There's very concerning data about safety with rosiglitazone. It's not definitive, but if TIDE is to provide that, we have many years before we're going to get that insight. We do have an alternative, pioglitazone, for which there is considerably strong safety experience. So I come down to, then, what is the continued role for rosiglitazone?
DR. THOMAS: Abraham Thomas. I voted E. The scientist in me says we should always seek the truth. But this isn't an NIH study section. This isn't the review of a journal for publication. Really, what this is is an intersection, as someone mentioned at lunch, between public policy and science. And when we look at it that way, we can't always have the absolute truth to make a decision. We have other classes that are available that we never had before for the treatment of diabetes. And if rosiglitazone was removed from the market, we still have another TZD, what has had a trial that does demonstrate no increased cardiovascular mortality, no increased cardiovascular events, in PROactive.